Our Community Health Workers play a valuable role in connecting underserved populations to the health and social services they need.
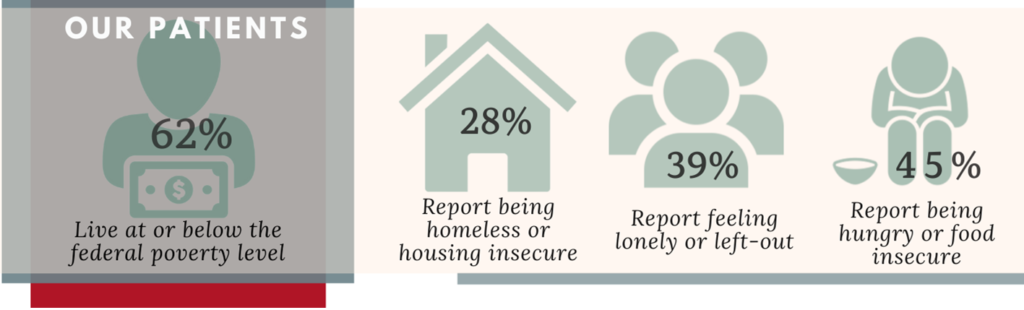
As part of our ongoing organizational improvement process, Sinclair Health Clinic’s Community Health Workers (CHWs) now manage enrollments as well as resource management patient cases. This enhancement improves our ability to immediately identify and assist patients with needs such as housing, food, and transportation. The info-graphic above was developed using information collected by the Clinic’s CHWs from nearly 500 new and renewing patients during the fourth quarter of 2020.
COMMUNITY HEALTH WORKER: A DEFINITION
Community health workers (CHWs) are lay members of the community who work either for pay or as volunteers in association with the local health care system in both urban and rural environments. CHWs usually share ethnicity, language, socioeconomic status, and life experiences with the community members they serve. They have been identified by many titles, such as community health advisors, lay health advocates, promotoras, outreach educators, community health representatives, peer health promoters, and peer health educators. CHWs offer interpretation and translation services, provide culturally appropriate health education and information, help people get the care they need, give informal counseling and guidance on health behaviors, advocate for individual and community health needs.
Since CHWs typically reside in the community they serve, they have the unique ability to bring information where it is needed most. They can reach community residents where they live, eat, play, work, and worship. CHWs are frontline agents of change, helping to reduce health disparities in underserved communities.
Among the many known outcomes of CHWs’ service are the following:
- Improved access to health care services.
- Increased health and screening.
- Better understanding between community members and the health and social service system.
- Enhanced communication between community members and health providers.
- Increased use of health care services.
- Improved adherence to health recommendations.
- Reduced need for emergency and specialty services.[1]
Sinclair Health Clinic has been at the forefront of CHW care in our area. Initiated in 2016, our CHW program continues to be refined and enhanced to better meet the specific needs of our patients and our community. In 2020 we expanded our CHW program, adding an additional Community Health Worker and focusing the CHW scope of work on enrollment matters and tracking and addressing needs identified through the social determinants of health survey, referrals from our providers, or direct outreach from our patients.
WHERE IT STARTS: SOCIAL DETERMINANTS OF HEALTH
Social determinants of health have been found responsible for 80% to 90% of health outcomes. An abundance of research has demonstrated that no matter the advancements in medicine and health care, individuals’ and communities’ health will not improve if these root-cause social factors are not addressed.
In 2020, the Clinic reorganized its CHW program, giving CHW’s the responsibility for collecting and assessing the social determinants of health surveys. Social Determinants of Health surveys are completed by both new patients during the enrollment process and, added in 2020, CHWs began capturing updated survey information from our existing patients during the annual patient recertification process
Now, with the real-time and updated survey information, the Clinic’s CHW’s can immediately make resource referrals, partner agency connections, and assistance applications for our patients instead of waiting until they meet with a primary care provider days or weeks later. This expedited level of support is demonstrating improved outcomes for those we serve.
HOUSING AND FOOD INSECURITY
Housing instability and food insecurity were both associated with measures of poor access to health care.
In research models, housing instability is associated with three outcomes:
- Not having a usual source of care
- Postponing needed health care
- Postponing needed medications
Food insecurity was associated with two outcomes:
- Delaying needed health care
- Postponing or skipping prescribed medications[2]
The Clinic’s Community Health Workers take immediate action with patients who indicate food insecurity. We refer patients to local food pantries, help patients register for local, state, and federal food assistance programs, and begin conversations about the underlying causes of the insecurity. 82% of patients connected to a food resource by CHW’s take advantage of that resource with 48-hours.
Similarly, the Clinic’s Community Health Workers assist patients indicating housing insecurity by connecting them to local organizations that work specifically on housing solutions. 43% of patients connected to a housing resource by our CHW’s take advantage of that resource within a week of referral. Internally, CHWs help patients take advantage of the many medication resources available from our pharmacy team, learn about the care available through our behavioral health team, and get scheduled with our clinic team.
Ensuring Sinclair Health Clinic patients understand and have access to every part of the Clinic’s professional healthcare team is what CHWs do best.
SOCIAL ISOLATION AND LONELINESS
The coronavirus disease 2019 (COVID-19) pandemic is highlighting one of these factors: social isolation. Social isolation, defined as an “objective deficit in the number of relationships with and frequency of contact with family, friends, and the community,” is associated with increased rates of the following conditions:
- Loneliness and suicide
- Hypertension
- Heart and kidney chronic disease.
- Demonstrated to be as dangerous to health as smoking 15 cigarettes per day.
Social isolation is identified as worthy of being a public health priority. A 2019 National Academies of Science, Engineering, and Medicine report, “Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health,” noted that being able to screen for patients’ social needs requires valid and reliable tools and the systems to help their use become routine. In addition to social isolation, screening tools should also focus on loneliness, which is different from social isolation. Loneliness arises from a discrepancy between desired and actual social connection level and is associated with detrimental health effects.[3]
In 2020, Sinclair Health Clinic, through our CHW program, added social isolation and loneliness screening questions to our Social Determinants of Health survey. Additionally, CHWs implemented strategies to begin the process of fully identifying and addressing social isolation and loneliness in our patients. Results to date are inconclusive, but progress is ongoing to effectively address the issues around social isolation.
TRANSPORTATION
Transportation barriers to health care have a disproportionate impact on individuals who are poor and who have chronic conditions. Studies document a significant problem in access to health care during a time of rapidly changing transportation technology. Studies found that Hispanic people, those living below the poverty threshold, Medicaid recipients, and people with a functional limitation had greater odds of reporting a transportation barrier.[4]
Sinclair Health Clinic CHWs address transportation needs in numerous ways. Where possible, we refer patients to local non-profit agencies providing transportation services. Additionally, we work with patients with Medicaid coverage to arrange transportation services through their managed care organization. Transportation is one of the more difficult issues to solve in our region; solutions are often complex, requiring numerous interactions with both the patient and transportation resources. The Clinic’s persistence has shown solid results. 73% of patients successfully have their transportation needs met when connected to a transportation resource by our CHWs.
WHY WE LOVE OUR CHWs
Access to healthcare services is critical to good health, yet many in our community face a variety of access barriers. Sinclair Health Clinic CHWs, Nuria Mendez, and Nina Castro as well as our numerous CHW volunteers, promote access to both the Clinic’s healthcare services and resources offered by our regional partners. The Clinic’s CHW team provides personal, bilingual, and caring support to help patients improve their health and enhance their overall quality of life.
[1] Role of Community Health Workers: NIH, 2014
[2] Housing Instability and Food Insecurity as Barriers to Health Care Among Low-Income Americans: J Gen Intern Med., 2006
[3] Social Isolation and Loneliness: Imperatives for Health Care in a Post-COVID World: JAMA, 2021
[4] Transportation Barriers to Health Care in the United States: Findings From the National Health Interview Survey, 1997–2017
